Laryngopharyngeal Reflux (LPR)/Silent Reflux Disease
Laryngopharyngeal Reflux is also known as LPR or Silent Reflux. The terms are interchangeable and you'll see all three used on this site. They have the same meaning.
Enquire about LPR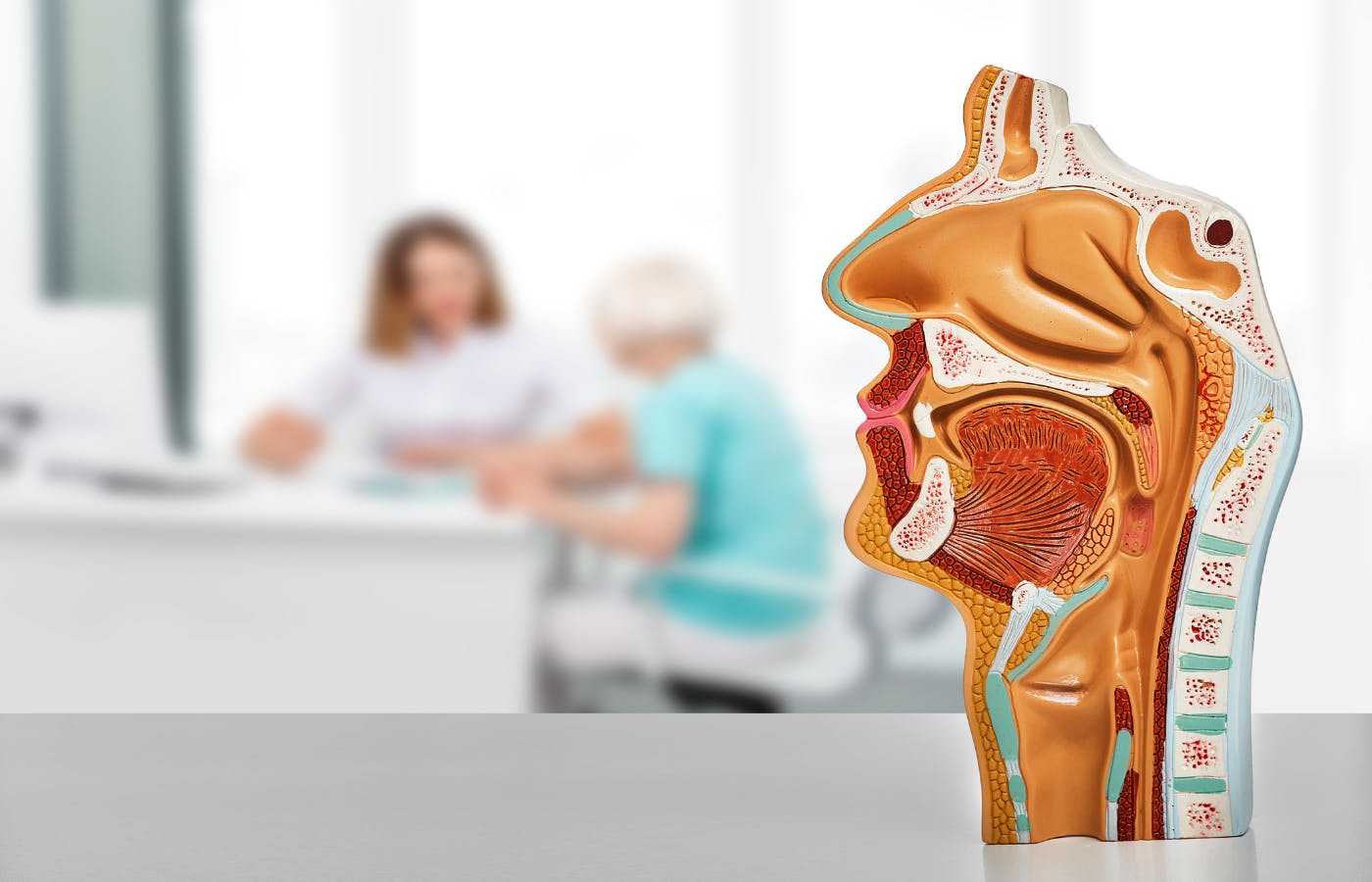
What is LPR?
There remains dispute among doctors as to what exactly LPR is and some even doubt its existence. There is no accepted scientific definition and it can be very difficult to both diagnose and treat. Signs and symptoms associated with LPR are however probably just as common as the heartburn/indigestion types and can be severe enough to blight some patients’ lives. Because so much remains unknown about LPR and the tests required to make the right diagnosis are not generally available, people often find themselves in what we call a “Cycle of Frustration”. However, since we see so many patients with LPR, as well as other reflux type symptoms, we have enormous experience and by using the RefluxUK MDT approach, as well as the most up to date tests and LPR treatment technologies we can achieve a good outcome for most people.
Laryngopharyngeal Reflux, or LPR, is often referred to as "Silent Reflux" - so what is "Silent Reflux" and why is it called that? Many of the traditional diagnostic tests will only measure acid reflux, while LPR is more often seen in patients with non-acidic reflux. As a result of this, clinicians will often say that the reflux is silent, or that a patient has silent reflux, as all tests come back negative.
At RefluxUK, we use state-of-the-art diagnostic testing to measure both acidic and non-acidic reflux.
Causes of LPR
So what causes silent reflux in adults? Throat symptoms can have multiple causes and it can be difficult to identify their exact cause. For instance throat clearing can be caused by reflux, a post-nasal drip secondary to allergies or sinusitis, vocal cord abnormalities, medications and can even be habitual. It’s likely that LPR can be caused by different problems and may well be more complex than simple GERD.
True LPR caused by conditions of the gastro-intestinal tract include;
- Gastro-oesophageal reflux disease caused by a poorly functioning Lower Oesophageal Sphincter (LOS); Failure of the LOS is usually associated with a hiatus hernia although in about 20% these are not identified. Reflux from the stomach can be in either liquid or aerosol/gaseous form and will cause local irritation or cause a nervous reflex for instance causing a cough. Importantly, the substances refluxing to the throat can be both acidic or only weekly acidic. It is thought that in particular an enzyme produced in the stomach called Pepsin can irritate the throat.
- Small Intestinal Bacterial Overgrowth (SIBO) ; Overgrowth of organisms within the small bowel that digest carbohydrates and produce gas can cause excessive belching/burping which in turn will cause reflux of gaseous reflux to the throat. Since SIBO can develop rapidly, LPR symptoms caused by SIBO can also be of rapid onset. Paradoxically, Proton Pump Inhibitors (PPIs) which are often prescribed to treat LPR symptoms are associated with SIBO and so may worsen rather than improve these.
- Gastroparesis / poor gastric emptying; if the stomach doesn’t empty properly either because of poor motility or a functional blockage then the pressure inside the stomach will exceed the LOS pressure causing reflux symptoms. Its literally like a damn across a river causing upstream pressure. In the case of gastroparesis in which the stomach nervous and muscular activity decreases symptoms can have a very sudden onset as it’s thought that viral infections particularly in young people are a common cause. Research also suggests that in some people there is a failure of the valve at the bottom of the stomach, the pylorus, to relax properly. In this case the stomach can’t empty properly as there is a functional blockage rather than poor muscular contraction.
- Oesophageal Inlet patch; There is evidence that in some patients a small patch of acid secreting tissue at the top of the oesophagus can cause irritation of the adjacent larynx and pharynx. This is also known as “hypertrophic gastric mucosa” and is probably an embryological remnant and so patients are born with the condition. Inlet patches are situated just beyond the upper oesophageal sphincter (UOS) and it is thought that as people get older and this weakens they can then start to cause symptoms. In some patients these may secrete mucous and on occasions can contain acid producing cells and so can cause inflammation and even ulcers at the top of the oesophagus. Research of Oesophageal Inlet patches is on-going.
- Upper oesophageal sphincter (UOS) dysfunction; the valve at the top of the oesophagus can become over-active in response to a failing LOS in an attempt to protect the airway. This may be responsible for LPR symptoms such as Globus. However, the role of the UOS in LPR remains unclear.
There are some authors that blame reflux on low stomach acid and suggest taking additional acid as a treatment. However, there is currenly no scientific evidence to support this theory.
What Symptoms Does LPR cause?
There are many symptoms of LPR or Silent Reflux and patients may have several or just one. Most often, they present in the throat, mouth, nasal cavity and lungs.
For more information on LPR Symptoms, follow the link below:
How is Laryngopharyngeal Reflux (LPR) diagnosed?
The cause of LPR symptoms are diagnosed by a combination of a clinician listening to a patient’s “history”, physical examination including visualisation of the throat and then diagnostic tests. These may be under the care of a throat specialist (usually an ENT surgeon) or reflux specialist. Ideally, since LPR can be a complex problem to diagnose and treat we recommend that this is ideally undertaken by experts from different clinical specialties working closely together (in a multi-disciplinary team).
The diagnosis of LPR is often made without any investigations of function and treated unsuccessfully on this basis. Formal reflux studies (see below) are often the key to reaching the right diagnosis.
Diagnostic LPR tests include;
- Laryngoscopy. These are techniques duing which a clinician, usually an ENT surgeon will examine the throat.
Indirect laryngoscopy: This uses a small mirror held at the back of your throat. The examining specialist will shine a light on the mirror to view the throat area.
Fiberoptic laryngoscopy (nasolaryngoscopy): This test employs a small flexible telescope. This is passed through your nose and into your throat after a local anaesthetic spray is used to numb the throat. This is the most common way that the voice box is examined. This procedure typically takes less than 1 minute.
Direct laryngoscopy: This employs a tube called a laryngoscope. This procedure allows the doctor to see deeper in the throat and to remove a foreign object or sample tissue for a biopsy. It is performed under general anaesthetic. - Gastroscopy: Otherwise known as upper GI endoscopy this involves inserting an endoscope through the mouth or nose into the oesophagus and then through the stomach and duodenum (together known as the “foregut”). The endoscope has a high definition camera enabling the operator to look for structural abnormalities such as hiatus hernias. They will also evaluate the lining of the foregut, for instance identifying oesophagitis, Barrett’s oesophagus and ulcers. If necessary samples of tissue (biopsies) can be taken for analysis. The examination can be performed with local anaesthetic spray, intra-venous sedation or under general anaesthetic.
- 24 hour catheter reflux monitoring. A small tube (catheter) is inserted through the nose to the bottom of the oesophagus and measures reflux events usually over 24 hours at the bottom as well as the top of the oesophagus. It will also include a pH sensor in the stomach to ensure normal acid production. The catheter is attached to a recorder about the size of a mobile phone and patients can record when they experience symptoms allowing correlation between the two. These are known as “symptom associations”. pH testing assesses acidic/non acidic reflux events. Modern testing includes impedance which offers the advantage that it also distinguishes between liquid, solid and gas reflux events. So for instance, impedance can identify belching and its relationship with reflux.
- Oesophageal pH capsule reflux test. The Bravo test involves attaching a tiny capsule during a gastroscopy onto the lining of the oesophagus just above the stomach. This records acid reflux over a period of 48-96 hours. Instead of a catheter it sends the data wirelessly to a recorder and falls off after the test is complete. The procedure is usually performed under conscious sedation.
- Salivary Pepsin. It is now possible to measure the concentration of Pepsin in the saliva. This may suggest evidence of GERD. However, while this test can be a useful indicator is not considered sufficiently accurate to definitively diagnose GERD. A negative tests does not rule reflux out while a positive test does not categorically confirm the diagnosis.
- SIBO/Intolerance Breath tests; breath tests are most commonly used to diagnose small intestinal bacterial overgrowth (SIBO) and malabsorption of sugars such as lactose or fructose. In the case of SIBO, following drinking a sugar solution the exhaled breath is tested over two hours to measure the production of hydrogen and methane gases by gut bacteria.
- Gastric Emptying Studies; These assess how quickly a substance passes from the stomach into the small bowel either directly using radio-isotopes (usually technetium-99m) or indirectly using breath tests. It can help diagnose gastroparesis or a blockage.
- Electrogastrogram; Delayed emptying can have many causes and measuring the electrical activity in the stomach can help distinguish them from each other. This can be done using electrodes placed on the skin and is painless and non-invasive.
What are the treatments for Laryngopharyngeal Reflux (LPR)?
Given the effect symptoms have on the sufferer's daily life it is understandable that there are so may patients out there seeking a cure. The most effective treatment for LPR is dependent upon identifying the cause. It’s not uncommon for patients to be given a diagnosis of LPR and treated on this basis with little benefit. Because so much remains unknown about LPR and the tests required to make the right diagnosis are not generally available, people often find themselves in what we call a “Cycle of Frustration”, often seeing multiple doctors without reaching resolution.
When SIBO is diagnosed, treatment will often abolish or improve symptoms.
SIBO treatments include;
- Identify and remove precipitants
- If PPIs provide no benefit stop
- Trigger food avoidance
- Low FODMAP diet
- Pro-biotics
- Anti-biotic eradication regimes
- Other diets. e.g. Elemental diet
GERD treatment
Lifestyle changes;
- Dietary changes such as eating smaller meals, avoiding trigger foods, eating earlier in the day
- Losing weight
- Stopping smoking
- Elevating the head of the bed at night
Medications;
- Alginates such as Gaviscon
- Simple anti-acids such as sodium bicarbonate
- H2 blockers such as Famotidine and Nizatadine
- Proton pump inhibitors (PPIs) such as Omeprazole and Nexium
- Others including Baclofen
Anti-reflux procedures;
- TIF
- Laparoscopic fundoplication
- Laparoscopic LINX
- Laparoscopic RefluxStop

Enquire about LPR
Fill out a simple contact form and we'll get back to you with next steps.
Get in touch